For anyone who is “vitamined-out” — ponder that the most important theme is not just about personally avoiding hospitalization, it’s Where the hell are our publicly funded universities? Does the Minister for Health serve the People, or Pfizer…
————————————–
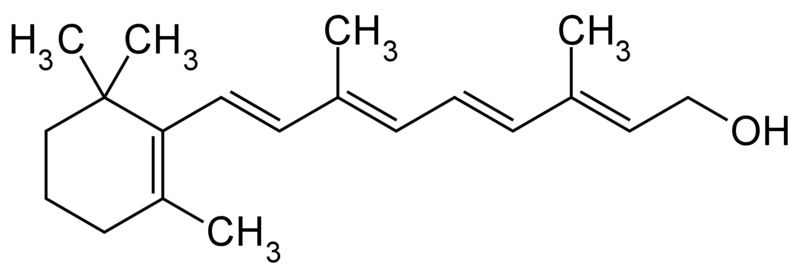
Vitamin A was allegedly once called “ “the anti-infective vitamin” — a snappy title which didn’t stick with any biochem student beyond the end of the sentence. But it’s needed for your immune system to function normally, so it seems sort of obvious to ask “what if” we don’t have enough. Could taking more prevent people catching Covid or ending up in hospital, or dead?
As always, research in prevention and prophylaxis is a wasteland in the the Modern West. No one can profit from it and indeed if everyone got enough it could harm the prospects of shareholders of Pharmaceutical firms and Hospitals. But it appears we definitely don’t want to be short of it. About three quarters of people who end up in the severe ward of Covid hospitals were deficient.
Imagine a Minister of Health who embarked on a program to raise awareness, test and give out free supplements? Lordy! It might reduce hospital loads in a week?

Vitamin A makes our bones stronger, reduces wrinkles, may prevent cancer and stops us going blind. But it’s possible to eat too much — especially if we dine out on polar bear livers or sled dogs. Seriously, overdosing for pregnant women causes birth defects and trouble for anyone who really overdoes it.
Sighs of Vitamin A deficiency include dry skin, excsma, dry eyes, night blindness, infertility, chest infections, poor would healing, and acne. Though all of these can be caused by other things too. People who are anaemic and people with inflammatory bowel disease, fibrosis, liver trouble or pancreatitis are more likely to be deficient.
Our immune systems can’t work without it
Our white blood cells that catch some booty (like body-parts of germs) will turn up to show it off, and when they do they’ll ooze versions of Vitamin A which induces other immune cells to respond to their prize and mature and proliferate. Vitamin A also manages to mobilize iron stocks to fill up the haemoglobulin molecules in baby red blood cells, something that makes them both red, and useful. It’s easy to imagine how extra red blood cells, and thus oxygen carrying capacity might be handy when dealing with a disease notorious for inducing low blood oxygen.

Vitamin A comes in meat, eggs and milk, but precursors (the carotenes) are found in leafy and colorful vegetables like spinach and carrots, so even vegetarians, in theory, ought to be getting enough of the building blocks so their livers can finish the job.
But a study in Spain showed that the sickest people with Covid were often the ones that were deficient. Three quarters of those admitted to hospital were deficient in zinc and Vitamin D, but nearly as many, 72%, were deficient in Vitamin A. And 42% were low in B6 (see Tomasa-Irriguible).
The problem with that kind of study is that we can’t be sure that the disease didn’t create the deficiency, and that the sickest people drained away their A and zinc in the process of getting sick. But from other studies we already know that Vitamin A is anti-inflammatory, as well as helping promote immunity. (Li et al) And that backing up a truck and giving super massive doses of 200,000IU to Covid patients appeared to save about two thirds of them from ending up with a severe disease. (see ).
Naturally, there aren’t many big good definitive studies in the West. We throw billions at patentable experiments, and our public universities, but no one is that interested in the ten-cent-nutrients that might reduce deaths by half. Though one large prospective study in the UK followed 15,000 people and found people taking Vitamin A and selenium supplements were quite a lot less likely to get a positive Covid result — odds were reduced by about 60% and 80%. (Holt et al).
One small Iranian study gave a mixed bag of vitamins to 30 patients and estimates the risk of hospitalization was 40% less, and the risk of death was 90% less compared with 30 “controls”. (It says something that we keep coming back to small Iranian studies, doesn’t it?)
That’s quite a bunch of vitamins used.
5,000 IU vitamin A daily, 600,000 IU vitamin D once, 300 IU of vitamin E twice a day, 500 mg vitamin C four times a day, and one ampule daily of B vitamins [thiamine nitrate [B1] 3.1 mg, sodium riboflavin phosphate 4.9 mg (corresponding to vitamin B2 3.6 mg), nicotinamide [B3] 40 mg, pyridoxine hydrochloride [B5] 4.9 mg (corresponding to vitamin B6 4.0 mg), sodium pantothenate [B6] 16.5 mg (corresponding to pantothenic acid 15 mg), sodium ascorbate 113 mg (corresponding to vitamin C 100 mg), biotin 60 μg, folic acid 400 μg, and cyanocobalamin [B12] 5 μg]. IRCT20200319046819N [1].
UPDATE: common vitamin names added [by me].
How useful is Vitamin A?
Just read the description of what vitamin A is used for in the immune system and try to imagine how well that will work in people who don’t have enough.
Vitamin A was initially coined “the anti-infective vitamin” because of its importance in the normal functioning of the immune system (23). The skin and mucosal cells, lining the airways, digestive tract, and urinary tract function as a barrier and form the body’s first line of defense against infection. Retinoic acid (RA) is produced by antigen-presenting cells (APCs), including macrophages and dendritic cells, found in these mucosal interfaces and associated lymph nodes. RA appears to act on dendritic cells themselves to regulate their differentiation, migration, and antigen-presenting capacity. In addition, the production of RA by APCs is required for the differentiation of naïve CD4 T-lymphocytes into induced regulatory T- lymphocytes (Tregs). Critical to the maintenance of mucosal integrity, the differentiation of Tregs is driven by all-trans-RA through RARα-mediated regulation of gene expression (see Regulation of gene expression). Also, during inflammation, all-trans-RA/RARα signaling pathway promotes the conversion of naïve CD4 T-lymphocytes into effector T-lymphocytes − type 1 helper T-cells (Th1) − (rather than into Tregs) and induces the production of proinflammatory cytokines by effector T-lymphocytes in response to infection. There is also substantial evidence to suggest that RA may help prevent the development of autoimmunity (reviewed in 24).
When deficient people get enough Vitamin A they also get more iron into their baby red blood cells.
…vitamin A supplementation in vitamin A deficient-individuals has been shown to increase hemoglobin concentrations. Additionally, vitamin A appears to facilitate the mobilization of iron from storage sites to the developing red blood cell for incorporation into hemoglobin, the oxygen carrier in red blood cells.
The RDA for adults is around 700 ug/day (women) and 900 ug/day (men). (That’s 2,333IU, and 3,000 IU). It’s worth being tested before embarking on a long term supplement program, but otherwise, having a bottle on hand for respiratory infections and short term dosing is probably a good idea.
For perspective: “Chronic toxicity results from daily intakes greater than 25,000 IU for 6 years or longer and more than 100,000 IU for 6 months or longer.” That’s quite a high dose. Be wary of pate made from bearded seals, polar bears, walruses and moose.
If you eat too many carrots, you’ll only turn orange. Plants are low risk.
Many studies were listed at the excellent https://c19early.com/va.
REFERENCES
Tomasa-Irriguible, T.-M.; Bielsa-Berrocal, L.; Bordejé-Laguna, L.; Tural-Llàcher, C.; Barallat, J.; Manresa-Domínguez, J.-M.; Torán-Monserrat, P. Low Levels of Few Micronutrients May Impact COVID-19 Disease Progression: An Observational Study on the First Wave. Metabolites 2021, 11, 565.
https://doi.org/10.3390/ metabo11090565
et al., EurAsian Journal of Biosciences, 14:7347-7350